Bridging the cancer care gap: Funding solutions for LMICs
Could targeted solutions, like a global diagnostics fund, ignite progress on NCD prevention, treatment, and care? Cary Adams of the Union for International Cancer Control weighs in on barriers to funding cancer care, innovative financing, and the critical role of political will.
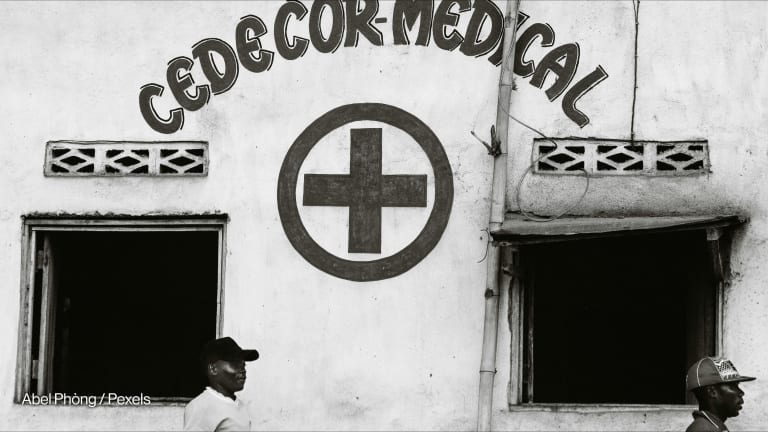
Despite being responsible for three-quarters of global deaths and placing a growing socioeconomic burden on governments worldwide, noncommunicable diseases, or NCDs, continue to receive only around 1%-2% of global financing investment for health. Progress in closing the NCD funding gap has been limited, despite numerous high-level United Nations meetings on the issue, with the economic impact of COVID-19 further hindering efforts, said Cary Adams, CEO of the Union for International Cancer Control. “There's a general acceptance across global health that NCDs and cancer were missed out in the [Millennium Development Goals],” explained Adams. “They are in the [Sustainable Development Goals], but the mechanisms of support are still very much focused on malaria, TB, HIV, and AIDS.” Meanwhile, in some low- and middle-income countries, the availability of cancer medicines, oncologists, radiotherapy machines, and pathology diagnoses capabilities is “appallingly low,” said Adams. UICC covers all aspects of cancer control and works to ensure that cancer continues to be a priority in the global health and development arena. By 2027, the organization aims to have secured a new commitment from the World Health Assembly on a cancer resolution and to reignite interest — on the tenth anniversary of the previous commitment — in tackling challenges in cancer control worldwide. While Adams believes the September 2025 high-level meeting on NCDs could be a turning point, he acknowledged that economic challenges will make progress in the coming years difficult. “Things can progress, but there are certainly some strong winds against us making rapid progress,” he said, “[particularly] in those parts of the world where the burden is increasing rapidly and the current health infrastructure is not mature enough to deal with that volume.” Devex spoke with Adams about the barriers to NCD investment and the steps needed for better global funding and planning to tackle chronic diseases. This conversation has been edited for length and clarity. What barriers are still preventing low- and middle-income countries and their governments from increasing NCD prevention, treatment, and care funding, particularly in the cancer space? Political will is critical to a country's response to its cancer burden. That often manifests itself in a national cancer control plan. There are more plans in place now than there were 15 years ago, and the quality has improved. But overall, we still haven't seen those plans implemented effectively and certainly, the funding has not come through. In LMICs, a significant proportion of the cost of cancer diagnosis, treatment, and care is out of pocket. There are methods for governments to pursue regarding insurance schemes and taxation, sin taxing, public-private partnerships, loans from the World Bank, and other development banks to invest in the core infrastructure required to provide some level of coverage for the more common cancers. It’s complicated, but there's a very willing international body of organizations there to help, or there's peer-to-peer help across countries. Where we have seen political will, for example in Rwanda, we have seen things happen. This reinforces the need that, at the high-level meeting on NCDs in New York next year, we get a strong political outcomes document that commits countries to take NCDs seriously for the next decade. How can public-private partnerships effectively address funding gaps, particularly in contexts where domestic resource mobilization is constrained? Public-private partnerships have a role to play, but they demand private capital, which is spread thin at the moment. In specific areas of health systems improvement, there is the opportunity to partner with the international private sector and tap into the capital markets. But with the current sovereign debt situation and the price of debt going up, that makes it really difficult to justify investment in some countries, given the need to secure a large return for the risk. So these partnerships have a role for some health infrastructure but, on their own, they're not going to address the challenges we're facing in cancer treatment and care globally. The other thing that's needed is bridging organizations that can provide some sort of guarantee or risk reduction, or put in capital where blended finance reduces the overall risk of the investment, but at the same time increases the return of the major investor. It demands partnership and the engagement of the likes of the World Bank and others, and for those providing sovereign debt and providing the capital to think imaginatively about how they can give more space to countries to invest in the core health infrastructure. Are there any examples of successful efforts to mobilize domestic resources and support sustainable health care solutions in LMICs? Rwanda is a good example of where there has been a significant change in the past 10 years. Again, where you have a country that has political will, that starts it all off. But I'm quite cautious to hold up a particular case study as an example because the nature of cancer in any country varies significantly in proportion to the other health challenges a particular country is undertaking, and in relation to what their current health infrastructure is and how they fund it. The context of a country should determine how they plan to address cancer in the future through a national cancer control plan. Within that context, there should be an agreed funding model. They roll out that model with the plan and over time become more in tune with their own cancer burden through introducing population-based registries. They can measure the impact of their policies and approach and refine those over time so it's more cost-effective and save more lives. There are case studies that are really useful, but fundamentally, a country needs to write its own plan. What would innovation in financing NDCs look like to you? The time for sin taxes to be called innovative has gone. That should be business as usual in every country and taxes on tobacco, sugary drinks, and alcohol should be in line with the World Health Organization’s recommendations. Where some innovation is needed is the current sovereign debt crisis in countries, because while that's not addressed, the fiscal space for investing in health is reduced. There are a series of innovative ways in which that debt can be restructured. We have seen it around climate change, where they have restructured the debt around a particular program at work to address climate change issues. They restructure the debt in terms of time of repayment, or into the cost of repayment if it's allocated to a specific economic issue within that country. We also need to get away from that annual discussion about having a global NCD or cancer fund in the same vein as the Global Fund to Fight AIDS, Tuberculosis and Malaria. There's no appetite in the current economic situation across multiple countries to have such a fund. But I believe there's an opportunity for us to come together on certain components that are critical in dealing with NCDs and cancer in LMICs. One I'm particularly passionate about is the ability to diagnose a disease and the pathology needed to fully understand what treatment is required to cure or treat that person. If we’re able to create a global fund for pathology and diagnostics, which allowed for every country that wants to improve NCD treatment and care to have those basics in place, that would be a step in the right direction. Maybe the innovation has to occur in how we're trying to solve the problem, rather than how we fund more money. Then, if you marry the solution with a funding solution, we're more likely to make progress. Visit Accelerating Action — a series highlighting pathways for funding NCD prevention and control, spotlighting innovative financing models and cross-sector collaborations. This content is produced in partnership as part of our Accelerating Action series. To learn more about this series, click here.
Despite being responsible for three-quarters of global deaths and placing a growing socioeconomic burden on governments worldwide, noncommunicable diseases, or NCDs, continue to receive only around 1%-2% of global financing investment for health.
Progress in closing the NCD funding gap has been limited, despite numerous high-level United Nations meetings on the issue, with the economic impact of COVID-19 further hindering efforts, said Cary Adams, CEO of the Union for International Cancer Control.
“There's a general acceptance across global health that NCDs and cancer were missed out in the [Millennium Development Goals],” explained Adams. “They are in the [Sustainable Development Goals], but the mechanisms of support are still very much focused on malaria, TB, HIV, and AIDS.”
This article is free to read - just register or sign in
Access news, newsletters, events and more.
Join usSign inPrinting articles to share with others is a breach of our terms and conditions and copyright policy. Please use the sharing options on the left side of the article. Devex Pro members may share up to 10 articles per month using the Pro share tool ( ).
For four years, Emma Smith covered careers and recruitment, among other topics, for Devex. She now freelances for Devex and has a special interest in mental health, immigration, and sexual and reproductive health. She holds a degree in journalism from Glasgow Caledonian University and a master’s in media and international conflict.