LONDON — Male contraceptive methods represent a “huge missed opportunity” for the development community both in terms of driving family planning and in helping to promote gender equality, advocates say.
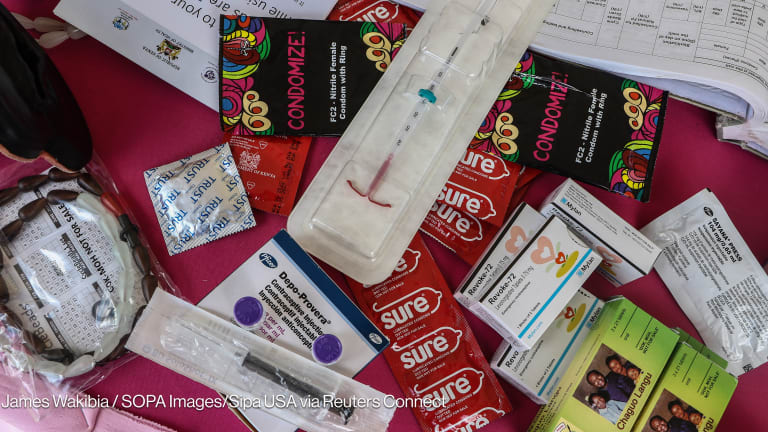
With access to family planning under threat from political opposition and funding cancellations, and an estimated 214 million women still lacking access to contraception, some advocates are making the case for increased focus and funding on male fertility methods such as vasectomy, a male contraceptive pill, hormonal gels, implants and injections.
They say the methods are typically overlooked by the medical and development sectors — but while the most commonly used male contraceptive, the male condom, is unreliable, innovative methods could drive family planning aims, including reducing unwanted pregnancies and improving child and maternal health rates.
Involving men can also lead to wider benefits, such as the promotion of gender equality, experts told Devex.
To date, family planning efforts have overwhelmingly focused on women and have included the development of new methods, such as the popular self-injectible Sayana Press. As a result, female usage rates have been steadily increasing, with the highest growth rates in Africa.
In contrast, attempts by pharmaceutical companies to develop male-centered contraceptive drugs and injections have largely been abandoned due to concerns about side-effects and the belief that there is no market. As a result, men’s choices remain limited to condoms, withdrawal and vasectomy, and studies show that male contraceptive usage rates have declined in recent years.
“If we look at the global data on contraceptive use over the last 20 years, men’s rates of use have barely shifted … [and] in some areas we’ve actually seen reduction … particularly in vasectomy,” Tim Shand, head of advocacy and partnerships at Promundo, an NGO that works to include men and boys as supporters of gender equality, said.
This negative trend matters not just because of the health risks and other complications associated with unwanted pregnancy for women, Shand explained, but also because it perpetuates the “current paradigm … which leaves the burden of responsibility of family planning on women and sees it as a women’s only problem,” he said.
But momentum for an increased role for men in family planning is growing, with additional funding going into the development of new contraceptive methods, alongside campaigns to raise awareness of the issue among men, their families, and policymakers.
Men’s growing role in family planning
Traditionally, birth control has been seen as a women’s issue. A UN study found that almost 60 percent of women in long-term relationships use the contraceptive pill or other form of modern contraception, with only eight per cent saying the male condom was the primary method.
Many men choose not to use male-oriented contraception due to “serious misconceptions,” such as a belief that it reduces sexual pleasure or can cause infertility, according to Shand, who added that having children is often an indicator of masculinity and so “men’s general objections to family planning … are strongly connected to male gender norms,” he said.
World Vasectomy Day, held on Friday, was launched in part to help challenge some of these norms by encouraging men who have decided not to have more children to get a vasectomy.
Now in its fifth year, the campaign’s centerpiece is a “vasectomy-thon” during which over 1,000 vasectomy providers from more than 50 countries carried out the procedure on an estimated 10,000 men, the campaign’s biggest turnout yet. The message is that the procedure is quick, easy and that it can be a beneficial decision for a man and his family.
Jonathan Stack, the American documentary filmmaker who co-founded World Vasectomy Day, said he was inspired to launch the campaign after making a film about a vasectomy doctor in Kenya. The experience challenged his assumptions about the procedure, he said, and he was surprised by what a “positive” experience it was for the men and their families, saying they “did it out of love for their family and children.”
It is not only men’s misconceptions about family planning that need to be challenged, said Stack, but also the family planning community’s. Many men are “really into having these conversations about family planning,” he said, and now is the time to harness the “aspirational energy” of today’s “more socially conscious” generations of men and women.
Untapped potential
Shand said that research by Promundo and others has revealed that “men will consistently say they have a desire to be more involved and supportive” when it comes to family planning decisions with their partner, but that traditionally the family planning community has tended “to see them as part of problem, not part of the solution,” and thus not invited them to participate. Family planning programs generally focus on women as the contraceptive users and ignore men as users in their own right.
Health systems and family planning policies are also structured in a way that tends to exclude men, he said. For example, vasectomy surgery is often unavailable and the healthcare environment is often “not conducive to men,” since it is based around “the more traditional women and child model.”
At a policy level, the Family Planning 2020 global campaign — which was launched in London in 2012 and committed a range of governments, foundations and companies to the target of ensuring 120 million more women and girls have access to family planning by 2020 — makes no mention of targeting men as either users or supportive partners, Shand pointed out.
“There’s untapped potential for men as users of family planning,” he said. That can be encouraged through greater communication around male-centered methods and education to debunk the misconceptions around both male and female contraception, he added.
Regine Sitruk-Ware, a distinguished scientist at Population Council’s Center for Biomedical Research and an expert in male contraception, agreed. “The family planning community has largely ignored men, but we remain committed to the notion that when presented with accurate and compelling information, many men will share responsibility for family planning,” she said.
Gains for gender equality
Advocates who spoke to Devex were clear that supporting more options for men should not come at the expense of efforts targeting women, but stressed the mutually beneficial nature of increasing choice for both sexes.
“By giving men better options everyone reaps the benefits,” said Aaron Hamlin, executive director of the Male Contraception Initiative (MCI), a private nonprofit foundation. He added that more options can “translate into better relationships, more gender equity, and fewer unplanned pregnancies.”
Shand described gender equality as the “untold story” behind programs that engage men to be supportive of family planning, referring to a Promundo and Rutgers MenCare+ program in Rwanda that provided men and their partners with a critical reflection and skill-building process around family planning, alongside other services, and that helped reduce levels of gender-based violence and led to improved communication and decision-making among couples. Thus, promoting male use of contraception can “provide an opportunity to think about a range of other issues linked to gender equality.”
Stack argued that there are currently too few family planning services for both men and women. He sees promoting male contraception as a “pragmatic” opportunity to create a change that should not come at the expense of women, he said: “I don’t think we need a counter women’s movement; we need a men’s movement to be better supporters of women,” he said.
The challenges
New products could help to drive higher uptake of male contraception, experts said, but until recently progress has stalled. Men currently have few choices, and nothing in the long-acting reversible category, Shand explained.
The biological differences between male and female fertility is one of the major challenges since, unlike women, men are essentially fertile all the time. That means hormonal interventions to stop sperm production need to rely on higher doses to be effective, and that can lead to more severe side effects.
In the past, pharmaceutical companies have explored expanding the market for men to include a male pill, injectables, and implants, but these efforts were dropped due to a perceived lack of demand and viability, according to Sitruk-Ware.
“Industry had withdrawn from this field based on the belief that men would not adhere to contraception as well as women do and because they did not see a large market for it,” she said. The “lack of regulatory guidelines on how to pursue approval for a male contraceptive” has also “cooled down” the interest of pharmaceutical companies.
David Sokal, chair of the MCI, added that drug companies have also been put off by concerns about liability. “Someone's going to get sick after taking the pill, and he's going to blame it on the pill, whether that's a true connection or just a coincidence,” he explained in an article for Vice.
Concerns about side effects are the main reason a 2008 study funded by the Bill & Melinda Gates Foundation and U.N. agencies on a male hormone-based injection was shelved in 2011 due to concerns about severe side effects and mood disorders and the fact that one of the participants committed suicide.
A Gates spokesperson told Devex that while the foundation has made some “innovation grants in male contraceptives to test the feasibility of making technical progress in a new area,” the foundation’s “primary focus is, and will continue to be, developing and distributing family planning methods to serve women’s reproductive health need.”
The opportunities
However, research and development is now being revived with new funding from the Gates Foundation and the U.S. government. New initiatives, including World Vasectomy Day and MCI, have also been launched in recent years to drive the agenda.
MCI’s Hamlin said the organization has provided grants for the development of male contraceptives that focus on non-hormonal reversible methods, which, instead of stopping sperm production, seek to prevent sperm from swimming or interfere with fertilization, for example.
“There's actually quite a lot of research in this space, though most of it is at the preclinical phase where they're still working on the chemistry or testing with an animal model,” Hamlin said. Gendarussa, a pill derived from an Indonesian shrub, is one of the efforts that is further along. It is due to start human clinical trials in 2018, he said.
Sitruk-Ware helped set up the International Consortium of Male Contraception, a network of doctors and professionals working on male fertility, in 2013. She said a number of new hormonal and nonhormonal contraceptive methods for men are under development. This includes Nestorone®/Testosterone gel, which decreases sperm production when applied. It is being developed by Population Council and the U.S. government’s National Institutes of Health.
A new product called Vasalgel, already being tested on humans in India under the name Rasug, could also be available soon, according to media reports. It works by injecting a gel into the sperm-carrying tubes that makes the sperm infertile, but is easily reversible with another shot.
Such advances mean a “male pill” could be closer than ever, Hamlin said — but getting these ready will require more funding.
“If we want to get a male contraceptive to market, then we have to provide significant funding for research in this early phase. Otherwise, a male contraceptive will never advance,” he said.
Greater advocacy around the importance of male contraceptives could help, Sitruk-Ware said, as well as research into “behavioral studies showing the willingness of men to adopt new methods in addition to vasectomy and condoms,” as this “may trigger more funding from donors,” she said.
However, new methods will be ineffective unless the international community is able to “change the conversation around men’s responsibility in family planning,” according to Shand.
“We need to shift the paradigm around this and build stronger commitment globally and nationally around men and [their role in] family planning,” he said. This needs to include a “focus on working with men and women around male gender norms and the benefits of using family planning for both men and their partners, and the broader benefits to gender equality as well as to communication and decision-making,” he said.
Read more Devex coverage on global health.