Global aid directed to the least developed countries reached a critical point in 2022, falling to its lowest level in a decade. That same year, member states of the Organisation for Economic Co-operation and Development’s Development Assistance Committee allocated only 0.37% of their gross national income to official development assistance — just over half of the Sustainable Development Goals’ target of 0.7%. As a result, more than 70 low- and middle-income countries — home to nearly 3 billion people — are bearing the consequences of this decline.
This setback was compounded by the abrupt withdrawal of foreign aid from Western governments earlier this year, leaving many LMICs grappling with a profound health financing crisis. As external funding continues to shrink and per capita health spending declines, we risk deepening global inequities and undermining years of progress in health and development. Today, governments face an urgent challenge: how to safeguard health gains and ensure future progress in the face of such formidable obstacles.
The answer is not simply more money. The challenge — and opportunity — lies in sustainable financing, especially for noncommunicable diseases, or NCDs, which are often deprioritized in times of economic upheaval. Yet NCDs are emerging as one of the greatest threats to Africa’s progress and prosperity.
The scale of the problem is breathtaking. In 2023, NCDs accounted for more than a third of all deaths in Africa, marking a 10% increase in less than a decade. In sub-Saharan Africa, individuals aged 30-70 face a greater than 20% chance of dying from a major NCD. The financial consequences are equally devastating. In 2016, NCDs were estimated to cost Ethiopia $1.1 billion, a burden likely echoed across the region as health systems and economies struggle under the compounded pressures of conflict, climate change, and escalating debt costs. Without immediate and sustained action, the crisis will only worsen. By 2030, NCDs are projected to surpass communicable, maternal, neonatal, and nutritional diseases combined as the leading cause of death in sub-Saharan Africa.
Amid this turmoil, there is hope. The shared challenge of NCD financing offers a unique opportunity to come together, share knowledge, and collaborate across borders. The Financing Accelerator Network for NCDs, or FAN, an initiative of the Access Accelerated-World Bank technical partnership, in collaboration with Results for Development, or R4D, is calling for a coordinated, regional approach to NCD financing, beginning with sub-Saharan Africa through its regional NCD Financing Accelerator, hosted by the African Institute for Development Policy, or AFIDEP.
A new report, “Health Financing for Noncommunicable Diseases: Landscape Analysis of Practices and Challenges in the Sub-Saharan Africa Region,” from FAN offers valuable insights into the NCD financing landscape across sub-Saharan Africa, anchored by case studies from six countries: Botswana, Ghana, Kenya, Rwanda, Senegal, and South Africa. Drawing on a desk review of key literature and policy documents across the region, as well as insights gathered from regional workshops and consultations with 18 government officials, policymakers, academics, financing experts, and civil society leaders, the report provides an analysis of current government and external expenditure on NCDs. It also identifies key NCD financing challenges and opportunities for learning and collaboration to strengthen NCD financing.
PATH and the Coalition for Access to NCD Medicines and Products — an Access Accelerated partner — are conducting a complementary country survey on NCD financing across more than 10 LMICs. This effort builds on and complements findings from the FAN NCD financing landscaping study in sub-Saharan Africa, aiming to strengthen coordination and support more effective investment in NCD responses.
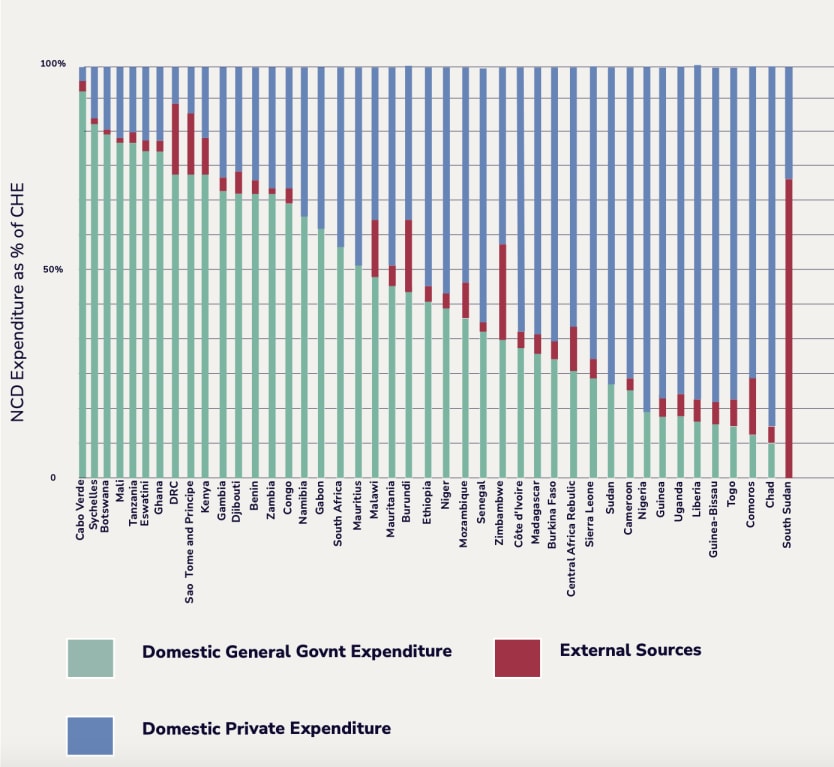
The findings reveal striking disparities in the allocation of resources for NCDs. On average, countries in the region allocate 23.5% of domestic government health expenditure to NCDs, but this varies dramatically, from 3.7% in Comoros to 50% in Eswatini. The variation is less stark when it comes to external health funding, where countries allocate an average of just 2.8% to NCDs, with figures ranging from 0.1% in Namibia to 10.2% in Guinea. While this is slightly higher than the estimated 1%-2% of official development assistance directed toward NCDs, it is still vastly inadequate. Taken together, government expenditure and external funding cover only an average of 47% of what people in sub-Saharan Africa are spending on NCDs, leaving individuals to shoulder the remaining costs out of pocket. The impact on patients’ and their families’ financial security can be catastrophic.
These disparities present a valuable opportunity to build a shared vision for financing NCDs and a collaborative approach to address the growing burden. By learning from successful approaches, sharing knowledge, and aligning priorities, countries can drive collective progress.
As African governments work toward greater financial independence, targeted support remains essential. Countries need technical support, stronger evidence, and platforms to optimize health financing for greater efficiency, sustainability, and equity. The solutions are clear but implementing them requires investment. So, what do these investments look like?
Consultations with stakeholders point to several priorities. Strengthening data systems is foundational. Timely and high-quality expenditure data are essential to identify, understand, and address financing gaps and to guide effective policymaking. Robust local data also helps build the evidence base needed to galvanize political commitment. When used to develop investment cases, it can clearly articulate returns on investment to policymakers, ministries of finance, and external donors.
Developing and implementing comprehensive NCD financing policies remain a priority for ministries of health, including efforts to strengthen and integrate national and private health insurance schemes, design effective benefits packages, test fit-for-purpose payment mechanisms for service providers, and identify appropriate service providers for various health services. Technical collaboration can also help establish coordinated procurement systems for medicines and diagnostic tools and support the implementation of innovative financing mechanisms such as health taxes.
Equally important is building the capacity to leverage private sector financing by fostering enabling environments for public-private partnerships and improving governance and accountability mechanisms across both sectors. Alongside these efforts, optimizing the broader health financing system remains key: from strengthening budgeting practices to addressing funding flow bottlenecks — ensuring resources are used efficiently and equitably for long-term sustainability.
FAN is committed to working alongside country members to build on the report’s findings and co-develop a clear road map for regional support. By aligning with country priorities and needs, we aim to help advance targeted, sustainable solutions that maximize impact on the ground.
As sub-Saharan Africa and the world navigate the current health financing crisis, ensuring sustainable financing for NCDs must be a top priority. This year presents a critical opportunity: at the fourth high-level meeting of the U.N. General Assembly on the prevention and control of NCDs, we must advocate for a greater focus on sustainable financing for NCDs. At the interactive multistakeholder hearing held on May 2, participants issued a clear and unified call: Governments must show stronger leadership and take bolder steps to invest in NCDs. As global leaders shape the future of the NCD agenda, it is essential to recognize that funding is not the end goal but a powerful and nonnegotiable means to save lives, strengthen economies, and build healthier, more resilient health systems for the future.
Visit Accelerating Action — a series highlighting pathways for funding NCD prevention and control, spotlighting innovative financing models and cross-sector collaborations.
This content is sponsored by Access Accelerated as part of our Accelerating Action series. To learn more about this series, click here.