Postpartum family planning — providing contraceptive information and access as a part of post-birth care — is a widely celebrated intervention. It’s been recommended as a “proven” practice by major institutions in the sexual and reproductive health space to address low levels of contraceptive uptake in the postpartum period, with evidence that it increases contraceptive uptake. However, a series of recent studies showing limited to no effects on rates of unintended pregnancy call its value into question.
Over the past year, my organization ran postpartum family planning programming in Ghana. In partnership with the Ghana Health Service, we integrated family planning counseling into postpartum care at 18 facilities across northern Ghana. We’ve since decided to shut down our operations: not because we lack funding, but because we don’t believe this work is sufficiently valuable to be worth our donors’ limited money and health workers’ valuable time.
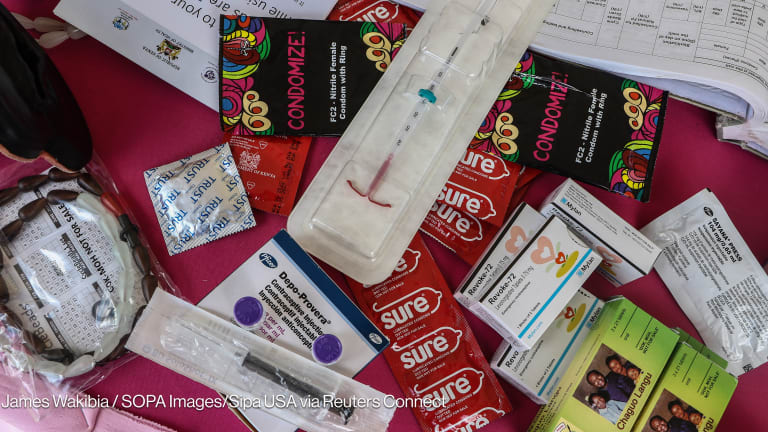
Proponents of postpartum family planning interventions cite low levels of contraceptive uptake in the postpartum period as a cause for significant concern. However, these numbers include only “modern” methods of contraception. When all kinds of protection are taken into account, a majority of African women are protected from pregnancy for an entire year postpartum.