Every country has a different starting point and pathway to universal health coverage. The aim for all countries — including low-income and conflict-affected states — is to make access to quality, affordable health services a reality for all people. The question of how to get there is often the most difficult to answer.
The first condition to achieving UHC is ensuring countries lead their own development and define their own priorities to address the health of their people. Government ownership, and partner alignment behind the countries’ specific contexts and changing needs, is essential to address the drivers and systemic challenges that will lead to improved access to quality and affordable health care.
“Political commitment and financing are not silver bullets … a rigorous focus on tracking results — and using those results to make evidence-based decisions and to course-correct — is key.”
—These challenges are being addressed in work being done across the global health community, that supports governments to bring together key partners to develop a national, prioritized health plan, called an investment case, and mobilize financing for the health and nutrition priorities in the investment case. This process helps governments make evidence-based decisions and align domestic and partner funding to finance priority health reforms. This approach also improves the current use of resources and strengthens the focus on results.
A look at GFF and UHC
The discussions set to take place at the United Nations High-Level Meeting on UHC are of critical importance to the goals of the Global Financing Facility, a partnership that was launched in 2015 when world leaders committed to achieving the Sustainable Development Goals. GFF supports low- and low-middle income countries to accelerate progress on health and nutrition, strengthening financing and primary health care systems for UHC.
A key focus in all countries supported by the Global Financing Facility, for example, is the delivery of a core package of maternal and child health services combined with key health system reforms to address the main bottlenecks in, for example, supply chains, or the availability and productivity of health workers.
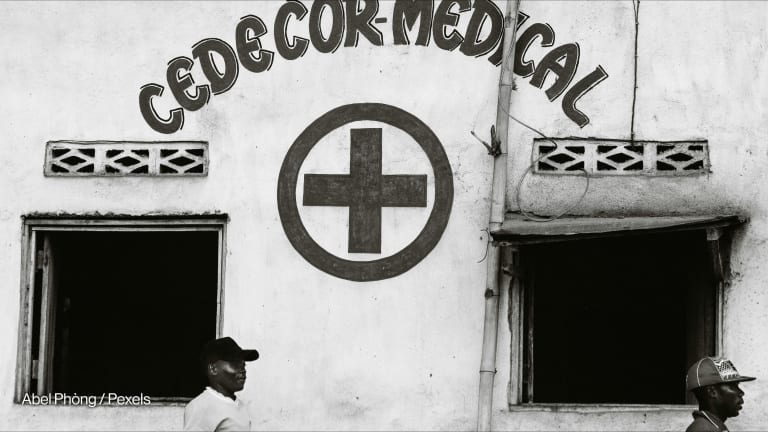
For example, the government of the Democratic Republic of the Congo prioritized the delivery and quality of a package of primary care services, as part of the investment case in combination with some core governance reforms, which allows for better use and alignment of domestic and partner funding. The initial results from 13 provinces show that these reforms have helped DRC make significant progress in improved patient access and affordability and increases in the delivery of reproductive, maternal, newborn, and child health services.
The second condition to achieving UHC is that available funding — both from domestic and external sources — needs to be prioritized to first address the needs of those left furthest behind, to fund high-impact services, and to address systemic bottlenecks. Too often, countries’ health strategies include interventions and services that are ambitious, but unfunded. For example, in 2014 Nigeria passed a national health act for a set of preventive, protective, promotive, curative, and rehabilitative health services or interventions.
A Basic Health Care Provision Fund, the principal funding vehicle, remained unfunded until 2016, when GFF funding was used to pilot the scheme in three states. Together with support from partners such as the World Bank and Bill & Melinda Gates Foundation, the government in 2018 decided to allocate 1% of its Consolidated Revenue Fund to finance the fund. A strong focus on quality as well as access, equity, affordability, and results — using available funding — is a key first step to lay the foundations to expand services and service coverage when the financing envelope for health increases.
Mark your calendar. On Tuesday, Sept. 24, Devex is convening a day-long UHC Pavilion on the sidelines of the U.N. General Assembly in New York City, hosting a series of events focused on the critical topic of universal health coverage. Sign up for the livestream on UHC here.
Primary health care is the arrowhead for transforming health systems to achieve the desired progress through high-impact, often neglected, services such as sexual and reproductive health and rights and nutrition. It lays a strong foundation for countries to achieve UHC in an equitable, and progressive way.
For example, the GFF partnership is supporting the government of Nigeria to expand access to health services to women, children, and adolescents in the northeast, a region affected by conflict that has historically been difficult to provide health services to. By creating incentives to improve maternal and child health outcomes, the region saw an overall increase in deliveries assisted by a skilled birth attendant and an increase in vaccine coverage from 2017 to 2018.
Political commitment and financing are not silver bullets. To translate into the desired impact, a rigorous focus on tracking results — and using those results to make evidence-based decisions and to course-correct — is key. Funds committed need to be on budget and tracked to the facility level and frontlines. This strengthens not only transparency and accountability but also allows governments to tackle bottlenecks, inefficiencies, and wastage.
As a global community, our work must be rooted in the needs and realities of the countries we support and address the real-world constraints and challenges governments face in ensuring health for all.
For a closer look at the innovative solutions designed to push for progress on universal health coverage around the globe, visit the Healthy Access series.