
For decades, the global narrative about health financing in Africa has remained largely unchanged: The continent is short on resources, reliant on external assistance, and vulnerable to donor priorities.
That narrative is now not only outdated, but dangerous.
Africa today stands at a crossroads. Global health architecture is fragmented. Disease threats — pandemics, climate-driven shocks, and noncommunicable diseases — are accelerating. Our population is rapidly growing. Public debt is rising. External assistance is declining sharply.
But even as these external crises converge, our greatest vulnerability in the area of health security is not a lack of funding — it is the failure to use existing resources effectively. Based on the Africa Centres for Disease Control and Prevention’s recently-released study regarding health financing on the continent, up to 40% of health spending is lost every year to inefficiency: fragmented planning, duplicative delivery systems, weak procurement, poor payroll management, ghost workers, and misaligned incentives. That level of waste would cripple even the wealthiest systems.
This inefficiency has entrenched dependency and undermined sovereignty. But inefficiency is not our destiny. It is not merely the result of individual decision; it is the product of systems designed by others and inherited over time. And those systems can — and must — be reimaged and rebuilt.
The real cost of fragmentation
Africa carries about 22% of the global burden of disease, yet accounts for only around 1% of global health expenditure. This imbalance is often cited as proof that Africa simply does not spend enough. But focusing only on spending levels misses the structural reality.
In many African countries, health systems operate through dozens — sometimes hundreds — of parallel plans, budgets, reporting frameworks, and delivery platforms, largely driven by donor financing. There are countries where ministries of health manage one plan, donors fund another, and implementing partners deliver a third. Each comes with its own timelines, indicators, data management systems, procurement processes, and accountability mechanisms.
The outcome is entirely predictable: duplication, administrative overload, leakage of funds, occurrence of fraud, and frontline workers stretched thin across competing priorities. Money is spent, but value is lost.
This fragmentation is not only inefficient but profoundly disempowering. It weakens national institutions, distorts policy priorities, and locks governments into short-term timelines that make planning beyond the next funding cycle impossible. In such a system, sovereignty cannot be achieved — no matter how much money flows in.
Efficiency is Africa’s new fiscal space
We now have the evidence to rewrite the script. According to the new study from Africa CDC, if African countries systematically address inefficiencies, they can recover approximately $14 per capita every year through better use of existing resources and some domestic reforms. That single figure is transformative: Within five years, it could be enough to replace roughly 50% of current donor financing for health across the continent and reduce dependence on external aid to below 20% of total health expenditure. At the same time, it would strengthen pandemic preparedness and response, improve service delivery, and expand financial protection to decrease out-of-pocket expenses.
This is not a theoretical exercise — rather, it points to action to unlock the value trapped in fragmented systems and put countries back in control of their health futures:
• Integrate national planning to replace overlapping strategies with one plan, one budget, one delivery mechanism, and one report.
• Pool the procurement of medicines and supplies, building on the African Pooled Procurement Mechanism approved by the African Union Assembly in 2024, to reduce prices by up to 30% while improving quality and transparency.
• Rationalize service delivery, especially through strong primary health care, reducing duplication and improving continuity of care.
• Digitize payrolls, logistics, and payments, eliminating ghost workers and financial leakage.
• Strengthen public financial management, ensuring that budgets are credible, predictable, and aligned with health outcomes.
Importantly, efficiency is not austerity. It is strategy grounded in practical reforms with proven results.
Dependency is no longer an option
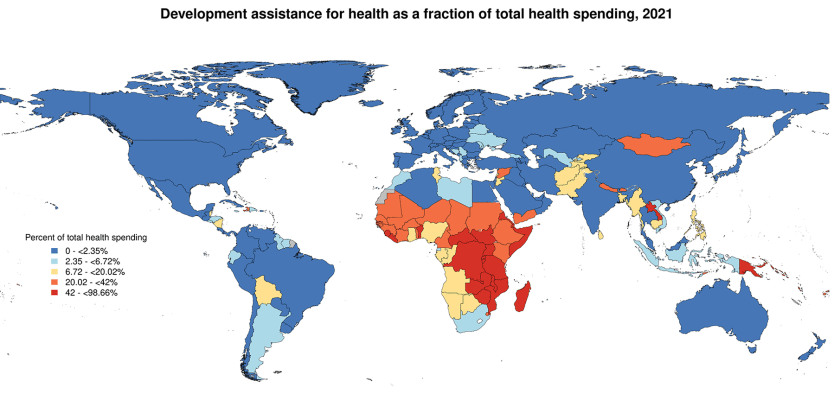
The model of fragmented, donor-dependent health financing is no longer viable. After peaking during COVID-19, official development assistance for health has declined sharply and is unlikely to return to previous levels. At the same time, more African countries are graduating from eligibility for concessional financing and disease-specific programs. This transition was always inevitable; it would be a mistake to treat it only as a crisis rather than an opportunity.
Continued dependence on external aid leaves African health systems exposed to volatility beyond their control. However, the answer is not disengagement from global partnerships, but a fundamental rebalancing of them: External financing should reinforce national plans, not fragment them; partners should invest through country systems, not around them. Accountability should be mutual, not asymmetric.
This is the thinking behind the “Accra Reset,” a reform agenda for the continent to move beyond aid and reclaim African leadership over development. It envisions moving from dependency to redesigned systems that deliver value for money in all sectors and putting country leadership back at the center with strong regional coordination.
While the “Accra Reset” sets the political direction, the Africa Health Security and Sovereignty framework, or AHSS, is the Africa CDC’s vehicle to deliver it via five pillars: reform of global health architecture, pandemic preparedness and response, sustainable health financing, local manufacturing of health commodities, and digital transformation.
By turning fragmented spending into coherent plans, stronger institutions, and better outcomes, AHSS reaffirms that Africa must have the ability to prevent, detect, and respond to crises without waiting for permission or pledges. True partnership begins with strong domestic stewardship — and leadership that is willing to redesign the system for resilience, sovereignty, and sustainability.
Health financing as sovereignty
Health is no longer a siloed social issue: It is a matter of national security, economic resilience, and political sovereignty. But sovereignty is impossible without stewardship. AHSS looks to institutionalize this stewardship by shifting the focus from spending more to spending smarter, governing better, and protecting households from catastrophic costs. It is about ensuring that every dollar, whether domestic or external, flows through accountable systems aligned with national priorities.
This approach unlocks broader gains. Efficient health systems reduce out-of-pocket spending, keep families out of poverty, improve workforce productivity, and build confidence between citizens and the state, strengthening the most valuable currency any government possesses — trust.
Africa’s future does not depend on charity. It depends on choices: discipline to cut waste, leadership to align partners behind national plans, and commitment to build institutions that finance health security sustainably. If we act now, the future of health in Africa will be defined not by scarcity, but by sovereignty, resilience, and shared prosperity.










