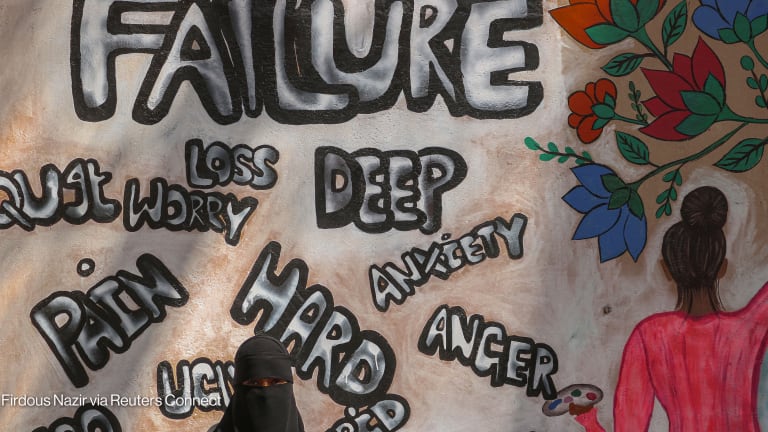
Lack of mental health and psychosocial support for people living with, or at risk of, HIV and tuberculosis, poses huge barriers to their health and well-being, as well as ending these epidemics.
This week, the board of the Global Fund to Fight AIDS, Tuberculosis and Malaria meets to discuss the fund’s strategy for the years to come. This is a unique opportunity to ensure that mental health — a missing piece in current strategies — becomes an integral part of the global responses to HIV and TB — from prevention, to testing, to treatment and care, and addressing stigma related to mental health, HIV, and TB.
On Oct. 10, World Mental Health Day, the Global Fund’s Executive Director Peter Sands stressed that mental health is inextricably linked with the fight against infectious diseases and indispensable to the fight against HIV, TB, and malaria.
We agree. Why? Largely because HIV, TB, and mental health are interrelated. Two decades of evidence shows that poor mental health is a risk factor for HIV and TB infections. Additionally, having HIV and/or TB is associated with developing mental health conditions.
It is … crucial that the Global Fund explicitly defines in its new strategy the importance of addressing mental health.
—The risk for depression is two and three times higher for people with HIV and TB than in the general population, respectively. In 2016, alcohol caused 254,000 deaths from TB and 33,000 from AIDS, representing 19.6% and 3.3% of all deaths from TB and AIDS, respectively. In addition, HIV has a broad impact on the nervous system and HIV-associated neurocognitive disorders — characterized by impairment in a set of cognitive, motor, and behavioral functions — often affecting adults living with HIV.
A body of research shows that individuals with mental health conditions and without care for those conditions have more limited access to testing and care for HIV and TB. When they are able to access care for HIV and TB, they are less likely to continue with treatment, leading to more severe disease and death from these diseases.
Watch:
► Achieving the SDGs: Delivering Mental Health for All
► Delivering mental health care for all: Why investment now is crucial
Furthermore, people with mental health conditions in mental hospitals and other institutions also lack access to HIV and TB testing and care. And there is also the burden of stigma, which is common to mental health conditions, HIV, and TB, and of double stigma associated with the comorbidities.
Integrating prevention and management of mental health conditions and psychosocial support within HIV and TB programs can therefore help improve people’s access to HIV and TB prevention and treatment, and their retention in care.
Strategies and programs that integrate interventions, services, and support for children, adolescents, adults, and older people, especially the most vulnerable, must form part of people-centred and human rights-based responses to the HIV and TB epidemics.
There is also a compelling economic case for integrating mental health with the HIV and TB responses. Every $1 invested in mental health, HIV, and TB programs can yield an economic return of $4, $6.40 and $43, respectively.
Integrating mental, neurological, and substance use disorder treatment into HIV and TB responses thus may synergistically increase those gains by improving health and well-being of affected people, reducing community transmission, and mitigating long-term catastrophic costs to individuals affected by these multimorbidities.
In practical terms, the World Health Organization’s Mental Health Gap Action Programme includes several evidence-based interventions that can be delivered effectively by non-mental health specialists with adequate training and supervision.
Such interventions could be widely introduced within HIV and TB programs. In addition, our two organizations are soon to introduce an implementation guide on integrating mental health and substance use services into HIV services. This would help guide countries in their efforts for integration.
What does all this mean for the Global Fund’s new strategy? It is imperative that the strategy lays the foundations for providing funding for mental health services at every stage of the HIV and TB service continuums as part of quality care and support. The upcoming board meeting is a vital opportunity to discuss mental health as an integrated part of the strategy.
In 2019, the Global Fund expanded its funding recommendations to include for mental health and substance use services. However, only a very small number of countries have included activities for integrating mental health and psychosocial support with HIV and TB interventions in their Global Fund funding requests.
It is therefore crucial that the Global Fund explicitly defines in its new strategy the importance of addressing mental health, and recommends specific types of mental health services and activities that countries could request funding for in support of ending their AIDS and TB epidemics.
The Global Fund has the opportunity to be a trailblazer by fully integrating mental health services throughout its programs. This will not only greatly strengthen systems for health, including community responses, but it will also, most importantly, bring better health and quality of life to countless people across the globe.