MANILA — HIV self-testing received an additional boost at the 22nd International AIDS Conference held last week in Amsterdam. Unitaid, one of its champions, announced two new projects promoting self-testing to a wider population in sub-Saharan Africa.
An estimated 75 percent of people living with HIV are aware of their status, according to latest statistics by the Joint United Nations Programme on HIV/AIDS. This is a significant leap from two years ago, when UNAIDS estimated 40 percent of people living with HIV remain undiagnosed.
See more coverage of AIDS 2018:
► AIDS 2018 told the story of a global health crisis
But concerns abound that such improvements are not seen in certain populations. In fact, latest statistics show an increase in new infections among high-risk groups, including men who have sex with men, people who inject drugs, sex workers and transgender people.
But an alternative to the current standard testing approach could help close the gap, creating a domino effect that would lead to more people getting on treatment and eventually, reduce their viral loads. Unitaid, together with its partners and several HIV experts and activists, is convinced that promoting self-testing could be the key.
“It’s not the only thing that will help close [the] gap, but we’re quite convinced that it will be a critical tool in helping to close it,” said Robert Matiru, Unitaid director of operations.
How much self-testing will impact the current numbers — and how far can it go to help meet the UNAIDS global targets set for 2020 — is currently hard to tell. But some initial evidence have shown promise, he said. In the initial phase of the HIV Self-Testing Africa Initiative the organization funded in 2015, they found groups of high-risk populations that had not undergone testing before, such as young men and sex workers, actually used the test.
“That first project basically proved in three countries in sub-Saharan Africa that self-testing is feasible, that it is acceptable, that it is safe, and that it is effective,” said the Unitaid official.
“HIV self-testing should be offered as an additional approach to HIV testing services. [strong recommendation, moderate quality of evidence.]”
— WHO Guideline Development GroupThey have used that evidence to convince the World Health Organization to introduce new guidelines recommending self-testing, which the health aid agency eventually did in 2016.
A WHO policy brief highlighted evidence of the approach contributing to an increase in HIV testing among men who have sex with men, and dispelled notions of potential social harms by people who test positive to HIV — an issue shared by some who are concerned of the lack of people’s immediate access to counseling following private diagnosis.
“Large-scale implementation in Africa showed that there were no incidents of self-harm, suicide, or adverse events with distribution of approximately 1 million self-tests,” Cheryl Johnson, WHO technical officer on key populations and innovative prevention, based in Geneva, told Devex. “WHO’s review of evidence found no identifiable increased risk in harm following HIVST compared to standard HIV testing.”
Additional data on the potential of social harm was presented at the AIDS 2018 conference, but she said evidence showed it was “very rare.”
In Vietnam, nearly 4,000 people participated in a pilot community-based HIV self-test done by the government in partnership with WHO in the provinces of Can Tho and Thai Nguyen in 2017-2018. No social harms were reported except for two individuals who experienced suicidal thoughts. But in his presentation at the conference, Van Nguyen, WHO technical officer on HIV and viral hepatitis based in Vietnam, said the two individuals received social support and eventually subscribed to treatment.
Despite this, country-wide implementation of self-testing remains low.
Mixed uptake
Affordability and linkage to care are also prominent concerns hindering implementation of HIV self-testing.
In the private sector market, pricing for HIV self-test kits can go as high as $48. In the public sector, including through NGOs, pricing for these products can range from $3-$15, at least for those that have received either regulatory approval, recommendation from the Unitaid and Global Fund-supported Expert Review Panel for Diagnostics, or WHO prequalification.
But in the past few years, several international organizations have made efforts in further bringing down the cost of these products, particularly for low- and middle-income countries. OraQuick HIV Self-Test, the first and only WHO pre-approved HIV self-test kit, is currently made more affordable under a $20 million partnership in 2017 between manufacturer OraSure Technologies and the Bill & Melinda Gates Foundation. That partnership has allowed OraSure to bring down the cost of the kit to $2 per test in 50 developing countries in Asia and Africa through governmental and nongovernmental organizations, excluding delivery, distribution costs, and taxes.
Currently, Unitaid is seeking to bring down test pricing and convince governments and international funders to invest in the approach, Matiru explained.
“We committed an additional $80 million to now position self-testing for scale up. By that, I mean completing effectiveness studies to show to governments and funders that investing in self-testing is a good use of [their] money … and secondly, to negotiate better pricing for tests and generate demand, making people, particularly young people, young men, and their partners aware that self-testing is safe, normal, and effective,” he said.
“So, a lot of our investment now are about getting better pricing, getting more companies to sell the product in the market, and getting people to actually seek and use the test,” he added.
Another concern is linkage to care. But trials presented in last week’s AIDS 2018 conference showed self-testing doesn’t have an effect on people’s initiation to treatment.
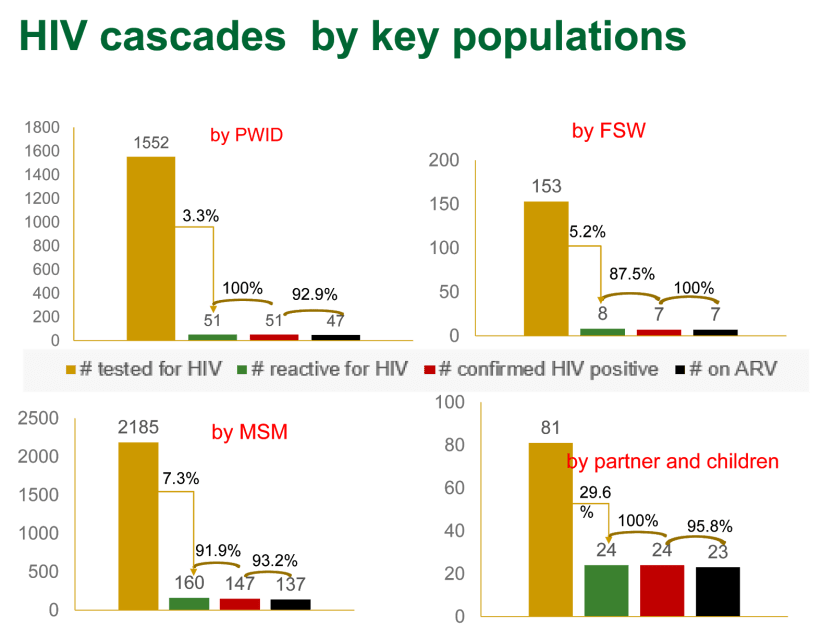
In Vietnam, a high percentage of people who undertook self-testing — either with the help of peer educators or alone — went on to confirm their status and signed on for antiretroviral treatment. But there were exceptions.
“You will see there are few people among [key populations] who did not go for confirmatory testing or ART. The first reason is that not every person [who] had reactive results after screening for HIV agreed or were ready to go for confirmatory testing or ART right after having tested or diagnosed. Sometimes, it takes several months. Thus, at any time point, there will be someone who needs time to accept their HIV status and to be ready for their lifelong treatment,” Nguyen said.
The others were unfortunately lost to follow-up or moved to another province, in which case they may have enrolled in an antiretroviral treatment site in their area of relocation, Nguyen said. They had one patient who died before being enrolled for treatment.
But policies and regulations play a critical role, too.
Since WHO’s release of the guidelines in 2016, 59 countries have developed policy on HIV self-testing. Many see this as a positive step, but to date, only 28 have made progress on implementation, according to data provided by Johnson. In 53 other countries, policy on HIV self-testing is still in development, while in 32 countries, WHO recorded either no policy, or the policy is still in development, or policy is being “piloted” and therefore not yet widely implemented.
In WHO’s Western Pacific region, only Vietnam is known to have a policy on HIV self-testing in action. China, which recorded the second largest number of people newly infected by HIV and AIDS-related deaths in countries in Asia-Pacific in 2017, has a policy in place but not yet widely implemented, although WHO has documented ongoing pilots in the country and four others, including Australia, Cambodia, Laos, and Malaysia.
Sixteen other countries in the region have “unknown” or no policy in place.
Policies are important precursors to introducing self-testing kits. They help open the market for self-testing, identify quality test kits that can be beneficial for the population, and define how self-testing should be rolled out and incorporated into national health care policies and testing strategies, among others.
But they can also impede its roll out and potential use. In Thailand for example, HIV testing is not allowed outside a health care facility. The government has also yet to approve a license for the use of OraQuick HIV Self-Test, which is manufactured in the United States and assembled in Thailand.
But with the traditional approach having at the limit of its effectiveness, especially in reaching high-risk populations, experts and advocates argue backing self-testing is worth the level of investment.
“Getting people notorious for not testing to come into public health facilities, to voluntarily come to testing centers to get tested, those have worked, but they’ve reached their limit. And particularly for those who don’t normally go there — young men, sex workers… men who have sex with men, transgender — they are not going to go to traditional points to get tested, because they are stigmatized, because it’s inconvenient, because it takes time out of their day,” Matiru said.
“Traditional approaches have worked for many, but they haven’t worked to put a dent on nontesting populations.”
