Enthusiasm for long acting reversible contraception, or LARC, methods, including implants and intrauterine devices, has grown dramatically among development and public health practitioners in recent years. Given their differential burden of early and unintended pregnancy, much of the effort to expand access to and use of LARC methods has focused on adolescent girls and young women.
However, scholars and advocates have increasingly cautioned against treating these methods as a “one size fits all” approach to reducing unintended pregnancy, and by extension, reducing socioeconomic inequities and poverty.
See more reproductive health stories:
► Could innovations in male contraception be the future of family planning?
► Work with women not for them, say advocates on World Contraception Day
► HIV, family planning groups grapple with new WHO guidance on popular contraceptive
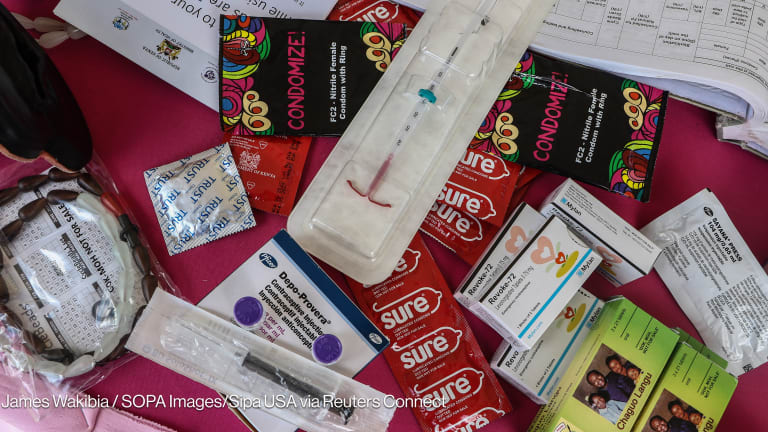
The prevention of unintended pregnancy benefits a wide spectrum of social, health, and economic outcomes for girls, their families, and their communities. IUDs and implants are the most effective reversible contraceptive options currently available. There are no contraindications to their use based on age or parity, and they do not require daily or monthly adherence. For many women, their use is associated with only minimal side effects — particularly as duration of use increases — and there is an option for a nonhormonal method, or Copper T. LARC methods can also be more convenient than other methods, as they may require fewer trips to the pharmacy or health clinic.
Despite these advantages, many women do not choose LARC methods. In high-income countries where information is readily available and fewer barriers to LARC access exist, such as product unavailability or lack of provider training, less than one third of women choose LARC, and usage among adolescent girls and young women is even lower: Only 5 percent of women aged 15-24 use LARC in the United States. The situation is similar in resource-constrained settings — most young women seeking a contraceptive method do not choose LARC. Even if LARC uptake in the least developed countries doubled, less than 10 percent of partnered women would use a LARC method.
Long-acting contraceptives are not always the best choice
In order to bridge remaining gaps in contraceptive services, it is important for us to recognize why LARC is not the answer for most women. First, effectiveness is not always a woman’s first priority. Rather, other factors may be more important in choosing a contraceptive method, including flexibility in starting and stopping a method, detectability, mode of administration — pill, injection, implant — minimizing side effects, and/or the need for dual protection against sexually transmitted infections, including HIV.
Second, despite its many benefits, LARC has disadvantages. Initiating a LARC method can be more expensive than other methods and requires a follow up visit for removal, and women also have concerns about the invasiveness of LARC placement, experiencing side effects, and having foreign objects or synthetic hormones in their bodies. Other women may want more temporary methods that can be removed without provider assistance and that enable a rapid return to fertility, especially if pressured to prove fertility upon marriage. Lastly, where heightened stigma surrounding adolescent sexuality and contraceptive use exists, confidentiality may be paramount. Although LARC is relatively discrete, the implant can be felt in the arm and IUD strings can sometimes be felt by a partner. Thus, the factors influencing contraceptive decision making are often complex and highly personal.
Development professionals must take a rights-based approach to contraceptive choice
Control of women’s bodies and their fertility has a long and unjust history. Lessons learned from the transgressions of the past such as the eugenics movement in the early 20th century and present, including forced sterilizations under national fertility limits, form the foundation of a rights-based approach to women’s contraceptive decision making. Power dynamics compound this legacy: In many places, adolescent girls and young women have less autonomy, financial independence, and freedom to access and decide to use contraception.
A rights-based approach to contraceptive choice was born from a need to respect and protect individuals’ choices about childbearing. This framework holds that people have the right to a “safe and dignified context” around the decision if and when to become a parent. Under this paradigm, women’s individual preferences and priorities should be at the center of contraceptive counseling, resulting in a method choice that is personally appropriate, not simply the most efficacious. For example, oral contraceptive pills and injectables may better fit the priorities of adolescent girls and young women while still being highly effective for preventing pregnancy, especially when coupled with strategies to promote their consistent use: Longer supplies of pills or the option for self-injection.
A rights-based approach to contraception does not prioritize LARC as automatically preferable to other methods, and ensures that contraception programs do not creep towards manipulation and/or coercion to adopt LARC or contraception in general. For example, some have advocated for a “LARC first” counseling strategy. Such an approach, coupled with an imbalance of power and information between providers and young women, may result in some women receiving methods that are inconsistent with their preferences. In this way, contraceptive counseling that prioritizes method effectiveness such as the World Health Organization tiered effectiveness model, although well-intentioned, may actually leave some women with a method not well suited to meet their needs. To achieve our ideal of the rights-based approach, development and health practitioners must allow the principles of equitable and balanced informed choice to play out.
How practitioners can incorporate rights-based family planning into their work
The simplest strategy is to ensure that women have a seat at the decision-making table. To develop effective programs for women, their voices and perspectives should inform every step of the process. This encompasses scientific leadership roles in the design and evaluation of new programs, contributions to the evidence base itself through participatory research models, and involvement in policy debate and creation. For example, when voluntary medical male circumcision was found to cut men’s risk of HIV in half, men’s perspectives were central in determining how to promote and increase access to this important prevention intervention. The benefits of circumcision to individual men — and not the known benefits to society or his partner — were at the forefront of these efforts. The same must happen with LARC. We must adopt a patient-centered approach and place an individual woman’s needs, preferences, and priorities at the starting point of the conversation — whether at the counseling table or within program design, evaluation, and policy creation.
In summary, we share in the excitement and promise of LARC for a variety of health and well being outcomes of interest to development professionals. At the same time, we recognize that there are legitimate reasons why women do not choose a LARC method. Especially among adolescent girls and young women who may prioritize factors other than method effectiveness and may face numerous other constraints, the balance may be tipped in favor of other methods. Although there is room to improve both supply and demand for LARC products, they are only one component of a healthy mix of contraceptive options, as evidenced by their low usage rates. To increase access and choice to all contraceptive methods while respecting women’s preferences and rights, a women-centered, reproductive justice approach is paramount. Each woman needs to be supported in identifying her health and life priorities and adopting the contraceptive method that best supports her needs.
Read more Devex coverage on reproductive health.