Health care providers in emerging economies understand that the pursuit of universal health coverage by 2030 will place considerable pressure on already over-burdened health systems. The fundamental challenge is that demand greatly outstrips supply.
Health care leaders operating at all points along the continuum of care understand that UHC by 2030 will require them to do a lot more with the same amount of resources. Fourth Industrial Revolution, or 4IR, technology, enables more efficient, effective management and implementation of health resources and interventions — this is where much of its application to achieving UHC by 2030 can be seen today. The real catalytic potential of 4IR technology — in combination with better management of resources — is its ability to fundamentally change models of care so that patients are empowered to take greater ownership of their health care, with a focus on prevention.
Real-world impact
The application of 4IR technology in overcoming the challenges of and ultimately achieving UHC 2030 is not hypothetical or a lofty ideal future state — it’s happening today. For example, learnings from a South African first in the fight against the HIV pandemic have built a strong foundation for 4IR and UHC by 2030 in South Africa’s public health sector.
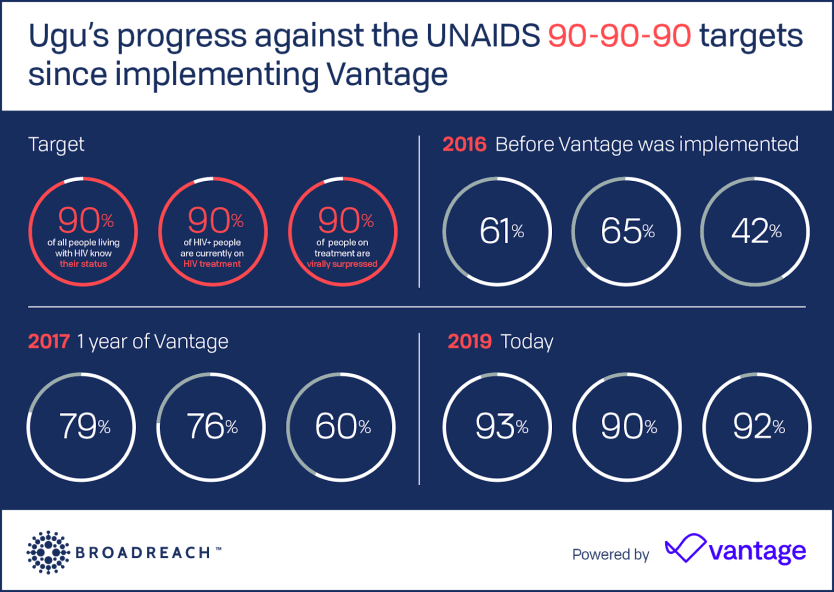
Working in partnership with the U.S. Agency for International Development, the U.S. President's Emergency Plan for AIDS Relief, and the Department of Health in Kwa-Zulu Natal, BroadReach Consulting applied 4IR technology to help them achieve the significant, resource-intensive feat of achieving UNAIDS’ 90-90-90 targets towards HIV epidemic control in the key district of Ugu.
By using Vantage — a 4IR analytics and workflow technology platform — Ugu has been able to manage the daily performance of individual health care workers and clinics. This has allowed Ugu to make real-time resource allocation and management decisions to boost performance. As recently as 2016, Ugu was widely considered the global epicenter of HIV, but a few weeks ago I took part — alongside Minister of Health Dr. Zweli Mkhize — in the celebration of achieving UNAIDS’ 90-90-90 targets.
“The application of 4IR technology in overcoming the challenges of and ultimately achieving UHC 2030 is not hypothetical or a lofty ideal future state — it’s happening today.”
— Dr. John Sargent, co-founder and co-CEO, BroadReachBased on this success, the KZN department of health is pioneering the way in achieving UHC using 4IR technology and has implemented Vantage to monitor and boost staff and clinic performance in both HIV and tuberculosis across the province, to cover hundreds of facilities and thousands of health workers. By expanding this work into other disease areas including noncommunicable diseases, health care providers can establish a strong first step in achieving UHC 2030. This achievement is a prime example of what UHC by 2030 looks like in real-world context.
Other real-world examples of 4IR technology changing the model of care and in so doing driving forward the UHC 2030 agenda include Zipline’s drone drug delivery, which makes medicines more accessible to people in hard to reach locations in countries like Rwanda and elsewhere. AI-powered apps such as Livongo and Babyl, which help people self-manage their chronic diseases easily and safely are also having an impact.
Data drives more effective management
As this example highlights, data, as it relates to a health program’s operations, is an invaluable resource; it can be used to optimize the way a health program is run and thereby increase the program’s impact in communities. It’s important to note that when thinking about data, the real value lies in extrapolating insights from the data and then proactively delivering predictive and prescriptive decision support customized to each individual stakeholder and assisting them to be much more effective in their work.
This is very different from the current practice of creating retrospective, descriptive, and passive visualizations and dashboards. We look at data as it relates to boosting individual decision-making and performance in several operational areas including workforce management and adaptive management. We find that working with data across interconnected operation areas enables more effective, systemic decision-making.
Adaptive management
Data-driven insight can provide both a broad and deep organizational oversight for leaders and — if captured in real-time and analyzed shortly thereafter, e.g. daily and weekly — it enables more dynamic management. If managers can identify program issues early, they can resolve them sooner and reduce the drain that these issues may have on health resources.
Predictive analytics is a fundamental driver of adaptive management. For example, our Patient Retention Best Practice, which uses predictive analytics to identify patients who are at risk of dropping off treatment, has been applied to a large-scale HIV program in South Africa with a patient base of 550,000 people. It has yielded predictive accuracy scores of between 80% and 88%, according to internal data, and allowed health care workers to feel empowered in intervening early and preventing patients from dropping off treatment — a far less resource-intensive job than trying to bring a patient back into treatment.
Workforce management
Workforce management is an obvious starting point when thinking about how to overcome the health resource burden.
Workforce management looks at how health care leaders can effectively manage large workforces to deliver quality care, at scale. Data-driven insight can be utilized to give management a consolidated view of what their entire workforce is doing and how they are tracking against achieving tasks and targets.
We leverage Vantage — AI-powered technology — to take workforce management one step further by providing program leaders with prescriptive recommendations for what each team member needs to do to contribute to the delivery of targets. We have seen great success in using this type of insight to help our clients spend their next hour more effectively.
4IR technology is by no means a “silver bullet” for solving the challenges of and achieving the ambitious and noble goal of UHC by 2030. However, they are certainly critical tools that will help health care leaders use their next dollar more efficiently and spend their next hour more effectively to deliver quality care to more people.