Four years on from the launch of the Sustainable Development Goals, average child mortality rates are falling almost everywhere. This is obviously great news. But new analysis from Save the Children suggests the underlying picture might be more problematic.
To go the next mile on child survival, development and government leaders will have to grapple with two big challenges: inequality and the role of public finance in addressing this.
As launched at the recent World Bank Spring Meetings, our report “Follow the Money” shows that while on average child health outcomes are improving worldwide, if you look at which groups are on track to meet the SDG goal of eradicating avoidable child mortality by 2030, gaping inequalities become apparent.
Perhaps unsurprisingly, the groups making the fastest gains are children in the upper-income quintiles. But, significantly, the poorest 20% of children are, in relative terms, just as far behind their richer peers as they were in the year 2000. And these inequalities are replicated across other identity markers, including gender, ethnicity, disability, and whether you live in a rural or urban area.
The family a child is born into is still the greatest predictor of their longevity and that should be a source of shame for leaders everywhere.
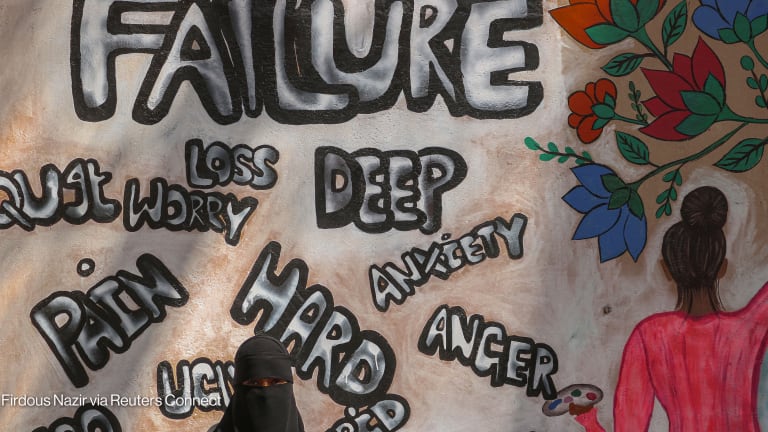
This astonishing failure to address health inequalities signals wider problems in the realization of the SDGs. The ambition of the SDGs, going much further than the Millennium Development Goals in committing to the eradication rather than the reduction of things such as child mortality, necessitates the SDGs most notable feature, which is the pledge to “leave no one behind.”
In order to achieve the goals, countries must achieve convergence between the groups furthest behind and the rest. In other words, the inherent logic of the SDGs is that the furthest behind must move fastest.
And it is this that is failing to happen, putting the goals at risk of ultimate failure. Our report shows that by 2030, on current trajectories, 4 million children under 5 will still die from treatable diseases, children drawn overwhelmingly from disadvantaged and marginalized groups.
This is a failure of leadership, prioritization, but also – crucially – funding.
Where leaders choose to direct public funds is a key driver of inequality. Yet, as was discussed at our event in Washington, D.C., inequality is not in turn driving the decisions of budget holders and finance ministries.
“Follow the Money” looks in detail at two countries — Kenya and Indonesia — to track the extent to which health budgets align to levels of health deprivation across different subnational areas and among different groups.
We found that, despite efforts by both countries to decentralize and introduce budget allocation formulas, there is an incredibly weak correlation between budget allocations and child health deprivation. This stands in opposition to the obvious fact that these children require a far greater share of public investment in order to catch up.
The poorest children are equally no more likely to benefit from core health services than their wealthier peers, in some cases less likely, despite far greater levels of need. Too often, the distance involved, out-of-pocket costs, or the inadequacy of available services prevent children from getting the care they need.
Without purposeful efforts to increase and direct scarce health resources toward the children and regions in the greatest need, and toward the types of primary health care services that most benefit the poor, countries will not see the convergence in health outcomes that must underpin overall SDG progress.
Addressing the scarcity and poor quality of budget and beneficiary data is a crucial first step, as is making better use of disaggregated data on health and nutrition outcomes. If we don’t know where the money’s going, or who needs it most, the game is lost before we begin. Save the Children’s Child Inequality Tracker shows how much we already know about the latter.
Global institutions and donors such as the U.K. Department for International Development have an important role to play here in supporting and incentivizing the development and use of much more granular data, for example through the World Bank’s Human Capital Project, and by making sure that aid-financed health services are transparent, equitable, and congruent with national budgeting and planning.
But the primary duty of ensuring every child’s right to adequate health and nutrition rests with their government, and in the provision of universal, well-designed, and appropriately funded services. It’s time for equity to be placed at the heart of health budgeting so that the commitment to leave no one behind becomes more than a noble intention.