
Since 2021, around 42,000 nurses have migrated from Nigeria to higher-income countries for better professional opportunities. Migration has also left the country with just 3.9 doctors per 10,000 people. Beyond migration, the limited focus on capacity building is another reason for the shortage of health care professionals in this country. Like Nigeria, many low- and middle-income countries, or LMICs, face the challenging shortage of skilled health care workers, further widening disparities in health care access.
The World Health Organization has predicted a shortfall of 11 million health care workers by 2030, mostly in LMICs. Within this workforce crisis, medical imaging professionals are critically in short supply. According to 2024 IAEA data, sub-Saharan Africa has only two radiologists per million people, compared to 93 per million in high-income countries.
Radiologists and radio technicians play a critical role in diagnosing and staging life-threatening diseases such as cancers, tuberculosis, and cardiovascular disorders. Furthermore, lack of access to essential and emergency surgical care is resulting in 17 million preventable deaths annually worldwide.
In many LMICs, equipment is often not fully utilized because of a lack of training; or even worse, sits idle because there is no one to operate it. Without proper training, purchased equipment provides little return on investment and becomes a further burden on the health care system.
Furthermore, underinvestment in health worker education and training continues to fuel workforce shortages. A holistic approach to capacity is crucial to address these challenges. Stakeholders must work together to introduce and scale innovative solutions in education and training.
Collaborations to access comprehensive curriculum
Rapid development of innovative technologies requires upskilling of staff, but many countries still lack structured training programs and faculty to support this skill development. Increasing workload on the existing healthcare staff is leading to burnout, manual errors, and creating bottlenecks in patient care, impacting the overall efficiency of healthcare systems. Addressing these challenges requires focused education, with resource integration from academia and industry.
To strengthen imaging diagnostics, countries can collaborate with organizations such as the American Society of Radiologic Technologists that develop radiology-related curricula as part of immersive training programs. Local health care providers can also partner with NGOs such as RAD-AID International, which offers hands-on training by experienced radiologists. Additionally, local radiology associations can work with online platforms to secure certified courses for their members.
By integrating structured, accessible, and scalable training into global health care education, these efforts help equip health care professionals in low-resource settings with the skills needed to improve patient outcomes.
Hub-level training centers for young professionals
Compared to a decade ago, governments are realizing the importance of education and training, but investments in these areas still require more attention. While the need for upskilling is widely recognized, access to training programs remains a challenge in many underserved regions. Moreover, health care workers often struggle to balance routine clinical demands with time for skill development. Setting up vendor-agnostic training centers at a regional level could offer a practical solution, ensuring accessible, standardized training without adding to the burden of daily clinical responsibilities.
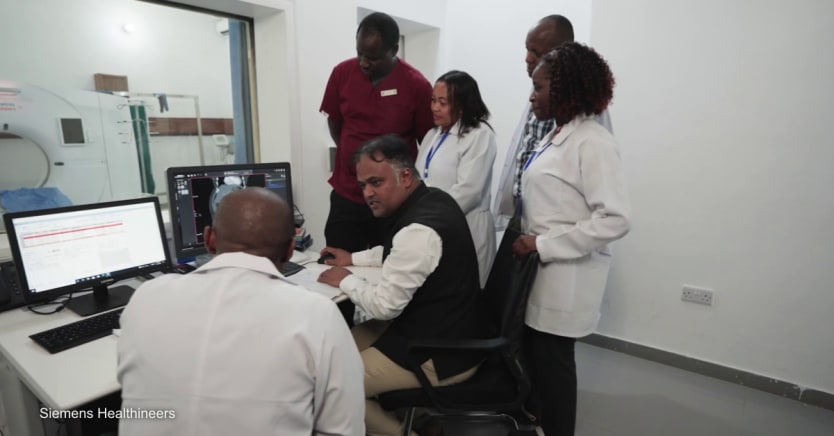
Such training centers can also be set up by universities and teaching hospitals. For example, the University of Cape Town in South Africa, in collaboration with various stakeholders, has been successfully driving radiotherapy training programs for over a decade to bridge the gap in radiotherapy education. Similarly, the Ministry of Health in Tanzania is collaborating with medtech leaders to upskill young medical imaging professionals, optimizing diagnostics knowledge and reducing patient waiting times.
Embracing digital solutions
Countries should take advantage of the digital-native younger generation because digitalization is key to improving the overall productivity of the health care staff. Technologies such as augmented reality, virtual reality, and 3D simulators now enable immersive training without missing out on the in-person training experience while adding a high level of convenience and environmental benefits.
Artificial intelligence, or AI, can also bring extraordinary benefits to resource-poor health institutions and is already a built-in component in many advanced medical systems. A collaborative approach integrating clinical radiology education, IT infrastructure, and AI deployment will help strengthen the radiology capabilities and better focus on patient outcomes.
A sustainable approach toward capacity building
Low-resource countries are increasingly focusing on building resilient health care systems in view of climate change, geopolitical issues, and rising inflation. Keeping people healthy is fundamental for driving economic growth and for capacity building to improve access and ensure the effective use of available technologies, education is key.
A future radiology technologist can work from home — it is already happening in some high- and middle-income countries to address staff shortages — but it can also be helpful to increase access and broaden expertise available to challenging geographies. While the lack of IT infrastructure and broadband are current roadblocks to adopting this concept in many resource-poor settings, if this trend accelerates, we could soon see technologists possibly working remotely on a nationwide or even international basis.
External factors such as migration, demographic changes, and the increasing disease burden are unstoppable. The pressing need is for long-term investments in scalable education and training programs. These initiatives have proven effective in bridging the global shortage of health care workforce.
Siemens Healthineers is contributing to addressing the workforce skills gap by providing education and training to health care professionals, supporting them to deliver high-quality care even in remote settings. The sustainability target is to provide 6 million hours of training by 2030. For more information, read Siemens Healthineers’ 2024 sustainability report.









