Mental illness affects one in four people in their lifetime and neuropsychiatric conditions now account for 13 percent of the global burden of disease — and 70 percent of that burden is in low- and middle-income countries.
Despite these figures, in both developing and developed countries across the world mental health does not receive the attention — or the funding — that it warrants. Although mental health problems account for almost a quarter of all the disability in the world, the poorest countries dedicate just 0.5 percent of their health budgets to it. Mental health was also notably absent from the Millennium Development Goals.
So how does a widespread health issue like this not achieve inclusion?
Given the statistics and the level of burden, you would be forgiven for thinking that achieving access and inclusion might be straightforward. However, it’s not as easy as it sounds. There are four characteristics of mental health that make it particularly hard to achieve inclusion or in other words, to turn the very real needs into simple policy realities and solutions.
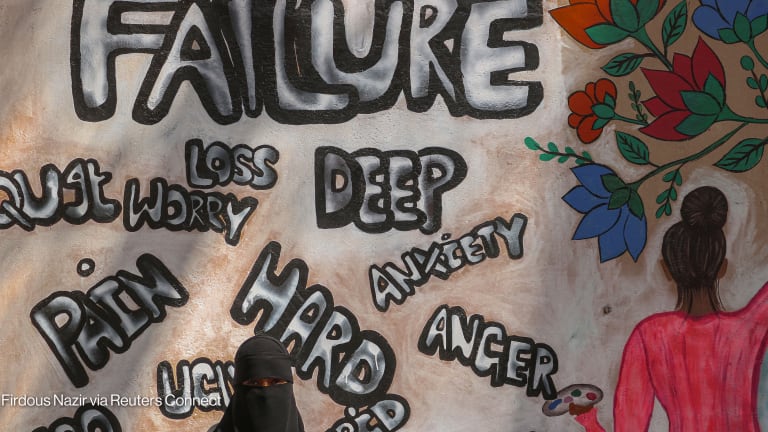
1. Policymakers are not immune to the huge stigma around mental health, which inevitably influences their treatment of the issue. Stigma is generally understood to be a combination of problems of knowledge (ignorance), attitudes (prejudice) and behavior (discrimination). While manifestations of stigma vary according to the mental illness and particular cultural context, they frequently result in an indifference by the public and policymakers to the needs of people suffering from mental illness and the inequities they face. This has meant that mental health is often absent from the policymaking agenda, or else that more general health policies exclude people with mental illness.
2. There are many types of mental, neurological and substance use disorders. Everyone’s experience is different — and so are the treatments they require. This diversity makes it difficult to develop a single, succinct ‘policy ask’ or promote one coherent solution.
3. Mental health isn’t like many other health issues such as HIV and AIDS — people with MNS disorders are only recently starting to unite into social movements. These movements haven’t yet been able to attract the kind of funding that has empowered the larger, better-known health movements to establish support systems and active global networks.
4. In low- and middle-income countries, a lot of mental health care is frequently provided in the informal sector, by family members or communities. Because it bypasses state systems it is effectively hidden. And all over the world, the underdiagnosis of mental illness leaves us with an inaccurate picture of the severity and scale of the problem. Consequently, the lack of evidence available on mental illness (much improved over the last decade or so thanks to the World Health Organization creating the World Mental Health Atlas) has made it harder to persuade policymakers to act.
There is hope, though, and inclusion may yet be on the horizon.
Public interest in mental health, particularly in high-income countries, has grown dramatically over the past 20 years. We are seeing real change at the intergovernmental level; at the 2013 World Health Assembly, 194 WHO member states committed to achieving the objectives and targets WHO’s Mental Health Action Plan 2013-2020. This milestone is a key opportunity for activists and practitioners to be heard and have influence. Networks like the Mental Health Innovation Network (funded by Grand Challenges Canada) can play a very important role shaping the way that the world reacts to mental health issues, with the projects they fund already finding cost-effective treatment solutions that can be applied in different countries, and rolled out to new communities.
This work is just starting, but will be crucial in coming years. This will help solve how mental health is included in a meaningful and lasting way.
The post-2015 sustainable development goals, now in the final stages of drafting, are a crucial opportunity to give access to those areas that are traditionally not included. Governments, international donors and the general public respond to high-level priorities like the SDGs, and campaigners (such as #FundaMentalSDG) are rightly calling for mental health to be included as a target.
If this momentum can be harnessed, the SDGs can be a formidable starting point to ensuring policymakers worldwide recognize the vital role that mental health plays in our daily lives. It would provide the cohesion, common framework and international governance structures to effect real change. It would be a way to get the ball rolling on inclusion and access for millions of people whose lives are affected by mental illness, and show that in the eyes of the international community, there can be no health without mental health.
Want to learn more? Check out the Healthy Means campaign site and tweet us using #HealthyMeans.
Healthy Means is an online conversation hosted by Devex in partnership with Concern Worldwide, Gavi, GlaxoSmithKline, International Federation of Pharmaceutical Manufacturers & Associations, International Federation of Red Cross and Red Crescent Societies, Johnson & Johnson and the United Nations Population Fund to showcase new ideas and ways we can work together to expand health care and live better lives.