With negotiations on the political declaration for the first U.N. High-level Meeting on Universal Health Coverage nearing conclusion in New York, many governments will be reflecting on what their commitment to “health for all” means back home. While their leaders have already signed on to numerous global health and sustainable development targets and commitments over the years, this September’s high-level meeting has ambitions to go beyond individual health issues.
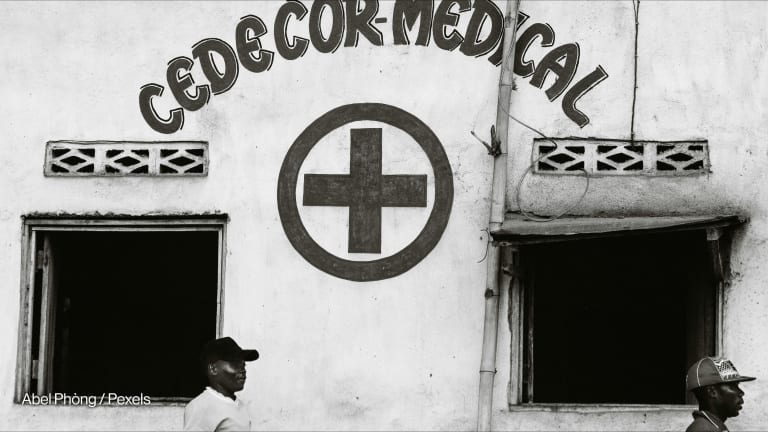
Defined as a situation where all people, everywhere, can access quality health services without incurring financial hardship, UHC has been described as the single most powerful concept that public health has to offer, and a key instrument to enhance sustainable development.
“In our collective pursuit to achieve healthy lives for all, we hear loud and clear that action-oriented solutions must be driven by meaningful involvement of those most affected, so that any risk of premature illness can be adequately mitigated.”
— Katie Dain, CEO, NCD AllianceWhile there is no “one size fits all” for national UHC responses — with countries embarking on different pathways tailored to their national contexts — noncommunicable diseases will be a key consideration for most countries, given the scale and geographic reach of NCDs. The sheer size of the burden, in terms of mortality and morbidity, makes these diseases impossible for governments to ignore.
NCDs also pose unique challenges and opportunities for the design and implementation of national UHC responses. Cancer, diabetes, cardiovascular disease, chronic respiratory diseases, and mental illness are chronic in nature, often lifelong, and people may live with two or more NCDs during their lifetime. For these reasons, they demand a fundamentally different type of health system from the acute care systems that prevail in many low- and middle-income countries.
The international development community has set a clear goal of reaching universal health coverage by 2030 — while leaving no one behind. How do we ensure access to quality care for all? This content series looks at the technology, practical solutions, and innovative financing tools driving improved access to quality care around the globe.
Major inequalities persist in terms of NCD risk, access to services, and health outcomes. The epidemic imposes a huge economic burden on national budgets, and too often pushes households into vicious cycles of poverty due to out-of-pocket payments. More than 60% of people living with NCDs have experienced catastrophic health expenditure, and this is most concentrated among the poorest and most marginalized populations in all countries, who are all too often left behind.
The NCD burden also presents a crucial opportunity for UHC: prevention. It is the foundation of primary health care, but it is an approach that has continuously — and regrettably — been sidelined in UHC debates. For some, prevention is a distraction from the core focus of UHC, which they deem to be strictly about treatment, care, and cure. However, this is extremely short-sighted, if not irresponsible. A large proportion of NCDs can be prevented or delayed.
Action can be taken by all governments around the world to stem the tide of NCDs and other health issues, avoiding the devastating human and financial cost these diseases impose on people, communities, health systems, and eventually economies.
So what does it mean to prioritize prevention within national UHC responses? What can governments do when they return from the high-level meeting to ensure health promotion and disease prevention is the first thought, rather than an after-thought, for UHC design and delivery?
1. Primary health care must be the foundation of all national UHC responses. PHC goes well beyond care and cure, encompassing the full continuum of care from promotion and prevention to treatment, rehabilitation, and palliative care. As the most common entry point for people to the health system, it can be instrumental in reducing health inequities and equipping individuals with the knowledge and tools to understand, participate, and actively manage their own health.
Mark your calendar. On Tuesday, Sept. 24, Devex is convening a day-long UHC Pavilion on the sidelines of the U.N. General Assembly in New York City, hosting a series of events focused on the critical topic of universal health coverage. Sign up for the livestream here.
In practice, for many LMICs, health systems will require substantial reform at primary care levels to better predict and prevent poor health, keeping people well for longer, with a higher quality of life, and needing to use the health system less and later in life. It will require wholesale transformation in some contexts. Zambia is a promising example, having recently implemented an integrative community PHC approach that focuses on prevention and promotion in order to help curb the rising tide of NCDs.
2. National UHC benefit packages must include proven, cost-effective prevention, and health promotion strategies for NCDs. Generally, health literacy is important across the board for prevention and health promotion — people must first understand health information and available services in order to make decisions that impact their health.
Vaccinations yield a substantial return on investment for devastatingly potent diseases: now even for NCDs such as cancer, there is exciting potential with the comprehensive rollout of human papillomavirus vaccines to eliminate cervical cancer. And, implementing evidence-based World Health Organization strategies for tackling modifiable risk factors such as tobacco, alcohol, unhealthy diets, physical inactivity, air pollution, among many others, has already saved millions of lives. Inclusion of these interventions is an important litmus test for a health system that is underpinned by PHC services spanning the full continuum of care.
More from Healthy Access:
► How voluntary licensing agreements are transforming HIV care
► Uzbekistan tests innovative financing model for hepatitis
► Opinion: Unlocking private capital to achieve 'health for all'
3. Public policies and action must be implemented across sectors. Without a sustained focus on the upstream drivers — social, commercial, and environmental — as well as modifiable risk factors of NCDs, UHC will drift out of reach for many populations. Leadership from the highest level of governments must implement evidence-informed public policies and mobilize action across all sectors as broad as education, agriculture, transportation, and trade to create health-promoting environments.
4. Consider policies to reduce consumption of unhealthy commodities. Adopting smart fiscal policies and pro-health taxes — for example tobacco, alcohol, and sugar-sweetened beverage taxes — not only reduces consumption of and exposure to unhealthy commodities, but has the dual benefit of providing a source of revenue for governments. Countries ranging from the Philippines, Egypt, and Thailand have leveraged unhealthy commodity taxes to support UHC schemes. This a win-win for health and economies.
5. Finally, and most importantly, we must listen to the people living with often multiple concurrent NCDs, to the communities most affected, to the children living in poverty, and the families working multiple jobs in polluted cities. In our collective pursuit to achieve healthy lives for all, we hear loud and clear that action-oriented solutions must be driven by meaningful involvement of those most affected, so that any risk of premature illness can be adequately mitigated.
People have had enough of environments that promote disease, disability, and disparity. Instead, we need environments that enable health, and it’s high time for governments to protect people’s fundamental right to healthy lives.
For a closer look at the innovative solutions designed to push for progress on universal health coverage around the globe, visit the Healthy Access series.

Search for articles
Most Read
- 1
- 2
- 3
- 4
- 5