When Michael Wheeler walked into a health facility in Birmingham, England seeking psychological support, he was turned away because of understaffing. Michael went home and continued to suffer — in the next few hours, he took his own life.
Across the globe, in Johannesburg, South Africa, Deborah Phehla was moved from a psychiatric facility to a community-based organization offering “sheltered housing” that didn’t have sufficient funding to provide for her basic needs. As a result, Deborah died of starvation, with horrific stories emerging of her eating plastic bags and scraps of paper out of sheer desperation.
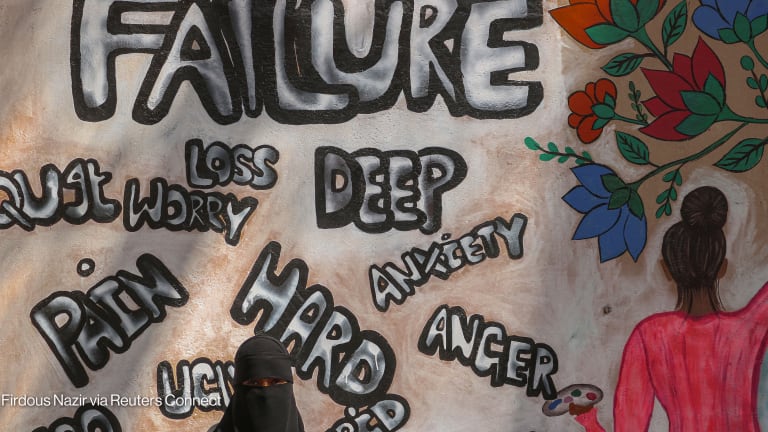
These entirely preventable tragedies illustrate the lack of resources for addressing the needs of people with lived experience of mental health challenges and underscore the reality of a global problem in need of urgent attention.