CANBERRA — Under the Millennium Development Goals, mental health was overlooked. But under the Sustainable Development Goals, goals for health include well-being. For advocates of better mental health support systems in developing countries, the goals are opening the door to build awareness on the diverse needs of people with mental health and the discrimination they face.
But despite changes, it is still progressing slowly — and in development assistance, mental health remains a low priority.
Dr. Julian Eaton, the senior mental health adviser for CBM, spoke to Devex on the importance of mental health and why there needs to be a greater focus from NGOs and donors.
Here is the interview, edited for length and clarity.
What are the fundamental reasons that mental health needs to be a greater priority in development?
Of people with disability, people with psychosocial disability are the poorest and the most unemployed in high income countries. The rates of unemployment among people with mental illness are almost 100 percent in many countries.
In low-income countries, the evidence isn’t so strong, but in a context with people with a more severe mental illness not being treated, it is very difficult to work anyway and people don’t trust you to work. They don’t give you work in the most rural places because you are thought to be possessed or contagious.
It’s partly the social justice issue of not employing people with a disability, but also it is not good for development. If 1 in 4 people in their lifetime have a mental health problem and if that is not dealt with properly, quickly, effectively, then it is likely to even affect their family’s income catastrophically. And it will also impact the capacity of a country’s economy to grow.
Development is held back by untreated mental illness.
What is the current state of mental health programming in development, including through development assistance?
Official development assistance needs to facilitate better mental health — it’s not front and center. But what do we really need to be doing?
“At the moment, the spending is scandalous and it is broadly encapsulated by stigma and ignorance. That must change.”
— Dr. Julian Eaton, senior mental health adviser for CBMOne of the things we spend a lot of time campaigning about in sub-Saharan Africa and the countries where I work is the pitiful contribution of money to mental health care — less than 1 percent of health budgets. And this is about the same amount from ODA’s health budgets directed to mental health.
That parity issue is really a very big advocacy point for us. There is no justification for this huge gap. Now it is just being out of date with evidence of appropriate intervention in low-income settings and the measurable impact that we know.
So at the moment, the spending is scandalous and it is broadly encapsulated by stigma and ignorance. That must change.
One of the things that has changed in the last 10 years or so is a recognition of all that we can do to support people with mental health issues. Previously there was an idea that even if we did have the money, it was still hopeless.
We have worked really hard on this to generate the evidence both of effective interventions and what the return on investment is. There has been a lot of really good work done recently, initially leading up to the World Bank spring meetings in 2016 which included mental health for the first time. And now it is being taken very seriously.
There is concrete evidence that packages costing $2 per year per person in low-resource setting create a return on investment of roughly 4 to 1. So the excuses are running out for not spending the appropriate amount on mental health.
The pressure is now on the donors to create the right level of impact in ODA toward mental health.
Is this attitude in development assistance out of tune with campaigns for mental health we see in developing countries?
The situation has changed very rapidly in donor countries. Australia, for example, is pioneering with Beyond Blue. But similar levels of awareness has been achieved in other countries, partly because of those campaigns and partly because the world is simply changing and people are speaking more openly about these things.
In the United Kingdom, mental health has become a cross-party consensus as a priority.
But the reason for the difference in developing countries is more due to a profound lack of understanding, lack of prioritization, and stigma in its broadest context. CBM has been doing mental health for 10 years now, but very few other organizations working in international development do mental health beyond the humanitarian sector.
Emerging best practices from Iraq for psychosocial support in emergencies
Frontline responders to the humanitarian crisis in Iraq say they are prioritizing psychosocial support in a way that hasn't happened in previous emergencies. Here are six of the best practices they've developed to help populations with overwhelming needs and limited resources.
The one area that is different is mental health and psychosocial support in emergency response, which is pretty well developed and always there and done OK. In longer term development, it is woefully inadequate — not many experts, not many departments, not many people who focus on that. And it’s a question of inertia largely.
A focus on mental health in humanitarian responses is important — but how does this assist with long-term mental health issues? Is there a point when mental health support is considered complete from the humanitarian side?
It’s very much a tick box exercise. On the positive side, it’s integrated, there are clear standards, but there is a tendency to tick a box.
First of all, there are people with severe mental illnesses whose support systems break down in an emergency — essential medication isn’t available and they’re even more likely to have a severe episode. And you have awful stories about psychiatric hospitals being left locked as all the staff run away during a tsunami.
The recognition of the long-term nature is problematic. Humanitarian assistance generally provides funding for three years and there isn’t a very good handover to the subsequent systems that take over.
One of the things CBM has done — pretty uniquely — in places such as Syria and Nigeria, is conduct health system strengthening as part of humanitarian responses. We have made sure, for example in Sierra Leone, that mental health services are in place to take up some of the longer term needs that have been exposed by Ebola or created by Ebola in the context of an extremely fragile health systems.
Emergencies create a lot of distress, but it is often the first time in a country that mental health has been raised as an important issue in health. Mental health systems need to be invested after an emergency and it is an opportunity to invest in them and to make systems better than they were before.
How do you prepare for and cater to the diverse mental health needs?
It’s something that is done pretty badly at the moment. Agencies tend to have one focus and history has created that problem.
Initially, there was a very strong push for treatment of posttraumatic stress for everyone in an emergency. That turned out to be really quite wrong and damaging — resilience is important and many people just needed help by talking to their neighbors and families and not to be stigmatized as mentally ill. And this also creates a big kickback against more comprehensive treatment for people with severe responses and the people with pre-existing conditions — people who have different needs from simply talking.
The big money that comes quickly just tends to do this basic support and assistance and no one is looking at those with more severe issues. We try hard to do that — we try to be very focused on health and strengthening, and in emergencies we try to look at that referral pathway.
I hope as the field develops, big agencies like Oxfam will start to have people who really know about mental health on staff — and not just the humanitarian psychosocial response. This will create a better linkage between the wider ranges of needs than there has been historically.
What is the progress that is being made on bringing a stronger focus on mental health in development programs?
We’re really supported by the huge progress that has been made at an international level over the last 10 or 15 years. There is a World Health Organization mental health action plan that has been passed at the very highest levels, including a body made up of ministers for health from all of these countries where we are advocating. So we’re able to feed back to them that they have signed up for this action.
The quality of resources from WHO and other organizations is so much better now and that has enabled local campaigners and local professionals to just really raise their game.
And there will be a global campaign for mental health bringing together major donors in a coordinated way to build awareness. And I have recently completed a scoping study for DFID [Department for International Development] and USAID [United States Agency for International Development] have appointed a mental health adviser for the first time ever — so the big agencies are starting to take this seriously now and I think it’s a matter time.
The thing that is starting to happen that will make the biggest difference is having the resources to help demonstrating change. That is something CBM has done a lot of — piloting programs in one district or region and taking that back to government who are the partners from the very beginning.
Creating systemic change is unlikely to be achieved by 2030. Realistically, what should we be aiming for?
There number one call by the movement for global mental health and people working in this sector number is treatment coverage. This is quite measurable because it’s within a structured sector — health. I think we need to be aiming for a substantial increase in coverage, especially for people with severe mental illness. And this should be seen in policy and accessible services.
Many countries are stuck with one national asylum where people are chained up — and you would never want to send a relative there. That profound change toward mental health care, including among primary health care, for people with mild to severe mental health illness is an important step and possible to achieve.
“Health systems must be a more dignified place to go.”
—At the same time it is not enough — it is not good enough. This is not just a health area. It is very tightly bound up in human rights and quality of life, and the second big ask of the movement for global mental health is related to human rights. Access to health care is part of that, but also the right not to be excluded from society.
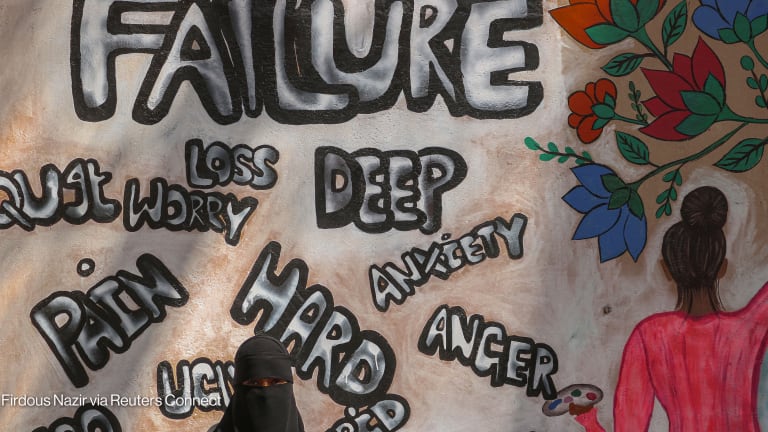
In many countries, their legislation clearly states people with a mental health condition cannot inherit property, they cannot vote, they cannot be a director of a board. These are institutionalized forms of discrimination.
The one that is perhaps measurable and changeable with intervention is people being systematically abused within government systems. Health systems must be a more dignified place to go. It has to be more dignified and responsive to needs, with people allowed to make decisions about their care rather than be authoritarian.
That must change. And subtle, daily discrimination in communities must also change.